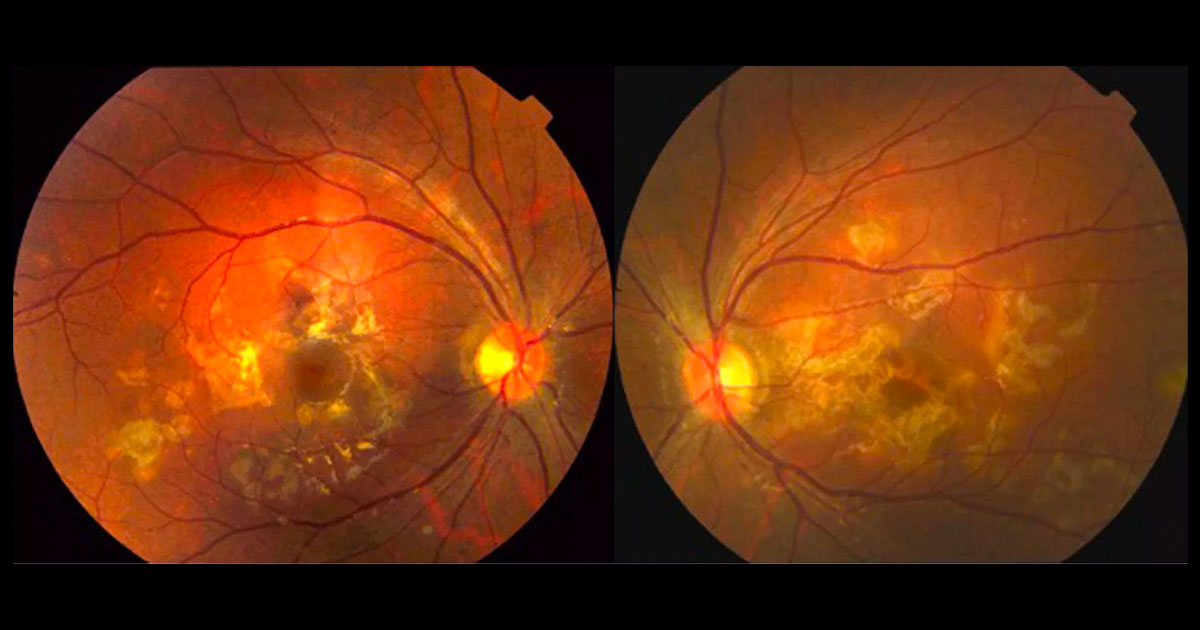
Figure 1. Colour fundus photographs showing multiple yellow-white deep retinal lesions at both posterior poles.
A 21-year-old male was referred with acute bilateral loss of central vision.
A 21-year-old male presented with a 2 week history of rapid bilateral reduction in central vision associated with photophobia and headache.
Six weeks previously he had been vaccinated, but he was otherwise healthy. He was born in India and had immigrated to Australia at the age of 3 years.
Visual acuity was 6/6 in the right eye (OD) and 6/36 in the left eye (OS). On examination there were 1+ cells in both anterior chambers, and a few cells in both vitreous humours. Multiple yellow-white outer retinal lesions were present at both maculae.
The differential diagnosis of multiple bilateral yellow-white deep macular lesions includes:
- Acute posterior multifocal placoid pigment epitheliopathy (APMPPE)
- Serpiginous choroiditis
- Multifocal choroiditis
- Sarcoidosis
- Tuberculosis
- Syphilis
Fluorescein angiography showed early hypofluorescence and late hyperfluorescence in the region of the lesions (Figure 2). Indocyanine green (ICG) angiography demonstrated hypocyanescence in the region of the lesions (Figure 3). Serum ACE, syphilis serology and Quantiferon gold were all negative. Brain magnetic resonance imaging did not show any cerebral vasculitis.
Figure 2. Fluorescein angiography of the left macula demonstrates early hypofluorescent and late hyperfluorescent lesions.
Figure 3. Indocyanine green angiography of the left macula demonstrates hypocyanescent lesions.
DIAGNOSIS
Acute posterior multifocal placoid pigment epitheliopathy (APMPPE).
Due to the acute loss of vision, the patient was prescribed a tapering dose of oral prednisone 70mg/day (1mg/kg). Vision improved to 6/4.5 both eyes after 6 weeks, although the patient has residual visual symptoms in the left eye due to foveal involvement. The macular lesions have started to pigment.
Acute posterior multifocal placoid pigment epitheliopathy (APMPPE) is an acquired inflammatory disorder affecting the retina, retinal pigment epithelium, and choroid of otherwise young healthy adults.(1) The disease is usually self-limited and is characterized by multiple bilateral yellow-white placoid lesions of the posterior pole (Figure 4).(1) Mild or no anterior inflammatory signs may be present. The lesions usually resolve over weeks to months, although pigmented scars may be visible. Recurrences may occur in up to 50% of cases. The degree of visual impairment depends on involvement of the fovea by a lesion, although 80% of patients maintain a visual acuity of 6/12 or better.(2)
The cause of APMPPE is unknown, but it is characterised by an occlusive vasculitis in the choroid, with secondary involvement of the overlying retinal pigment epithelium (RPE) and outer retina. This produces characteristic angiographic appearances. On fluorescein angiography there is early hypofluorescence reflecting choroidal non-perfusion and late hyperfluorescence due to inflammatory involvement of the RPE and outer retina, with breakdown of the blood-retina barrier. On ICG the lesions are hypocyanescent, reflecting choroidal non-perfusion.(3) Systemic vasculitis can also occur.(4,5)
There is a wide differential for APMPPE, as the differential diagnosis above shows. It is important to consider both infective and inflammatory causes. Cross reactivity with viral antigens is postulated to explain why the disease is often seen in association with a recent viral illness or vaccination.6
In most cases of APMPPE, the lesions resolve spontaneously, and no specific treatment is required. Steroid therapy is considered for those situations where the fovea is involved or threatened, or when there is associated systemic vasculitis.
Figure 4. Deep yellow-white placoid lesions characteristic of APMPPE.
TAKE HOME POINTS
- Acute posterior multifocal placoid pigment epitheliopathy (APMPPE) is a rare inflammatory condition characterized by multiple bilateral deep placoid lesions in the posterior pole.
- It is most commonly seen in healthy young adults, although there may be a history of recent viral illness or vaccination.
- It usually resolves spontaneously and overall has a favourable prognosis if the fovea is not involved.
REFERENCES
- Gass JD. Acute posterior multifocal placoid pigment epitheliopathy. Archives of ophthalmology 1968;80:177-85.
- Cheung CM, Yeo IY, Koh A. Photoreceptor changes in acute and resolved acute posterior multifocal placoid pigment epitheliopathy documented by spectral-domain optical coherence tomography. Archives of ophthalmology 2010;128:644-6.
- Howe LJ, Woon H, Graham EM, Fitzke F, Bhandari A, Marshall J. Choroidal hypoperfusion in acute posterior multifocal placoid pigment epitheliopathy. An indocyanine green angiography study. Ophthalmology 1995;102:790-8.
- Hsu CT, Harlan JB, Goldberg MF, Dunn JP. Acute posterior multifocal placoid pigment epitheliopathy associated with a systemic necrotizing vasculitis. Retina 2003;23:64-8.
- O’Halloran HS, Berger JR, Lee WB, et al. Acute multifocal placoid pigment epitheliopathy and central nervous system involvement: nine new cases and a review of the literature. Ophthalmology 2001;108:861-8.
- Baxter KR, Opremcak EM. Panretinal acute multifocal placoid pigment epitheliopathy: a novel posterior uveitis syndrome with HLA-A3 and HLA-C7 association. Journal of ophthalmic inflammation and infection 2013;3:29.
Tags: bilateral vision loss, photophobia, acute posterior multifocal placoid pigment epitheliopathy, serpiginous choroiditis