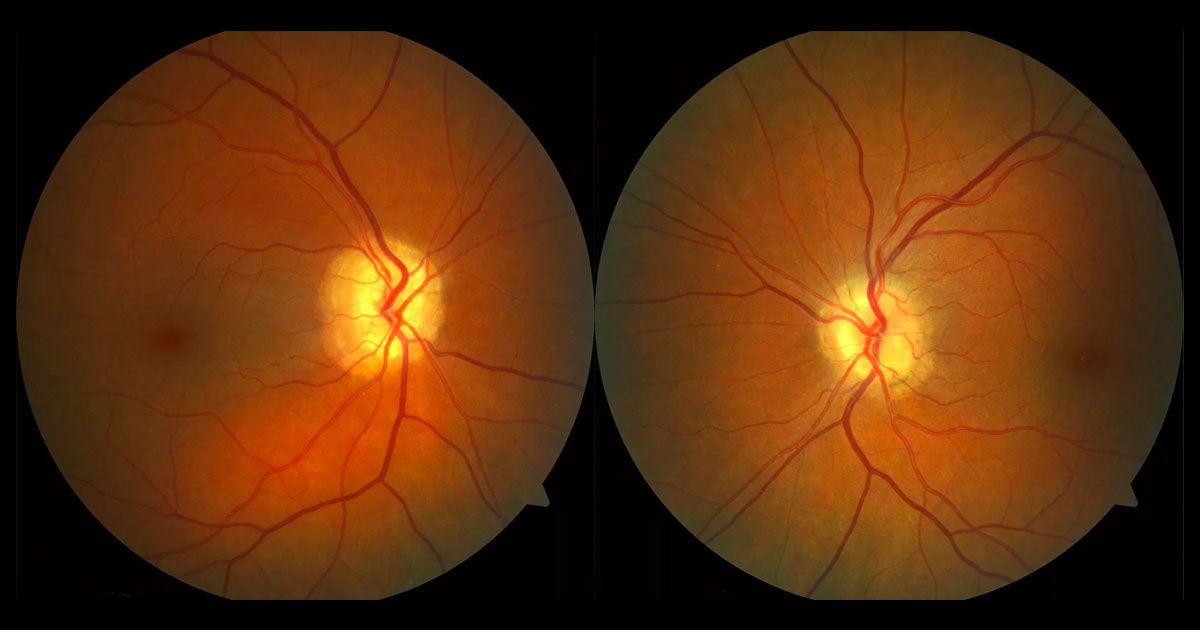
Figure 1. Prominent optic discs are seen in both eyes with small cup:disc ratios.
A 46-year-old lady was referred by her optometrist with an abnormal optic disc appearance and flashes in her right eye.
A 46-year-old lady was referred by her optometrist with abnormal optic disc appearances and flashes in her right temporal visual field over the last 2 weeks. These flashes were most noticeable when she viewed a white wall or bright light. Past medical history included breast carcinoma treated with surgery, chemotherapy and radiation.
The patient was a low hypermetrope. Visual acuity was 6/6 in the right eye (OD) and 6/5 in the left eye (OS). Intraocular pressures were 23mmHg OD and 22mmHg OS and central corneal thicknesses were normal. Anterior segment examination was normal. Fundus examination demonstrated a prominent optic discs without blurring of the disc margins, haemorrhage, lipid or subretinal fluid (Figure 1). Cup:disc ratios were 0.1 in each eye. The posterior hyaloids were still attached. Maculae and retinal peripheries were normal with no evidence of a retinal break.
The differential diagnosis of prominent optic discs includes:
A) Optic disc swelling (papillitis)
- Papilloedema (disc swelling due to raised intracranial pressure)
- Optic neuritis
- Neuroretinitis
B) Pseudo (apparent) optic disc swelling
Blood pressure as measured in the rooms was normal. Fundus autofluorescence showed marked hyperautofluorescence within the optic discs (Figure 2). Optical coherence tomography (OCT) scans through the optic discs showed a granular appearance (Figure 3). OCT of the retinal nerve fibre layer (OCT RNFL) showed thinning superior and inferiorly in the right eye and inferiorly in the left (Figure 4). A B-scan ultrasound showed hyper-reflectivity with shadowing at the optic disc (Figure 5). Humphrey visual fields (HVF) showed a superonasal scotoma in the right eye and nasal step in the left (Figure 6).
Figure 2. Fundus autofluorescence shows marked hyperautofluorescence at the optic discs.
Figure 3. Optical coherence tomography of the right optic disc shows a granular appearance within the nerve.
Figure 4. OCT RNFL shows thinning superior and inferiorly in the right eye and inferiorly in the left
Figure 5. B-scan ultrasound shows a hyper-reflective mass at the optic nerve head.
Figure 6. Humphrey visual field testing shows a superonasal scotoma in the right eye and nasal step in the left.
DIAGNOSIS
Optic nerve head drusen.
The diagnosis was explained to the patient and she was reassured that both the optic nerve head drusen and flashes were benign. Despite elevated intraocular pressures and changes on the OCT RNFL and HVF there were no clinical signs of glaucoma on optic nerve head assessment. It was presumed that the OCT RFNL and HVF changes were secondary to the optic nerve head drusen. The patient was asked to return in 3 months for repeat intraocular pressure testing, as ocular hypertension remains a possibility. Symptoms of retinal detachment (an increase in flashes, floaters or visual field defect) were described and the patient advised to present immediately if these occurred.
Optic disc drusen are hyaline, calcified bodies found in the optic nerve head anterior to the lamina cribrosa.(1,2) They may be visible at the surface or buried within the nerve head, and are often associated with anomalous tortuous, branching or looping retinal vessels.(1) The prevalence has been reported as 0.2-2.4%.(1,3) Although most cases occur in isolation, they may also be associated with retinitis pigmentosa, pseudoxanthoma elasticum and Alagille syndrome.(1)
Symptoms occur in approximately 50% of cases, and may include visual field loss and/or changes in visual acuity.(1) Visual field loss is more commonly associated with visible than buried drusen, and when there is concomitant ocular hypertension,(4) as seen in the patient presented. The most common scotomas are inferonasal sectoral and inferoarcuate.(1) Larger drusen and those that occupy a greater area of the optic canal are associated with more retinal nerve fibre layer abnormalities.(2) Visual acuity defects are mild, with 98% of patients having a vision of 6/9 or better, but optic disc drusen can cause transient visual obscurations.(1) In addition to the drusen affecting vision themselves (presumably due to axonal compression), they may be associated with choroidal neovascularisation, retinal vascular occlusions and haemorrhage.(2)
Differentiating between optic disc drusen and true causes of optic disc swelling (papillitis) is extremely important. Features that may suggest papillitis include:(5)
- Hyperaemia or pallor.
- Blurring of the optic disc margins.
- Retinal vessel obscuration, dilatation and telangiectasia.
- Optic disc haemorrhages, cotton wool spots, lipid, oedema and/or subretinal fluid.
- Paton’s lines (circumferential peripapillary retinal folds).
- Lack of spontaneous venous pulsations.
- Symptoms and signs of raised intracranial pressure (headache worse when lying down and in the morning, nausea and vomiting, decreased consciousness, diplopia etc.).
- Leakage on fluorescein angiography.(6)
The presence of optic disc drusen can be confirmed by multimodal imaging. Monochromatic photography may have a higher sensitivity and specificity than colour fundus photography.(7) Fundus autofluorescence shows marked hyperautofluorescence, due to the presence of extracellular mitochondria.2 Enhanced-depth imaging optical coherence tomography (EDI-OCT) shows the drusen as hyporeflective tumefactions bordered by hyperreflective material,(2,4) but the appearance can be variable8. Traditionally, B-scan ultrasonography has been the gold-standard for detection of optic disc drusen.(4) This shows brightly echodense lesions within the optic nerve head due to calcium within the drusen.(9) A similar hyperdensity can be seen on computed tomography (CT) scans.
TAKE HOME POINTS
- Optic disc drusen are hyaline bodies found in the optic nerve.
- They may be visible or buried.
- Although generally benign, they may be associated with visual field defects and mild visual acuity changes.
- Differentiating optic disc drusen from true optic disc swelling is extremely important.
- Key investigations that can assist in the diagnosis include optical coherence tomography, fundus autofluorescence and B-scan ultrasonography.
REFERENCES
- Wilkins JM, Pomeranz HD. Visual manifestations of visible and buried optic disc drusen. Journal of Neuro-Ophthalmology 2004;24:125-9.
- Sato T, Mrejen S, Spaide RF. Multimodal imaging of optic disc drusen. American Journal of Ophthalmology 2013;156:275-82.e1.
- You QS, Xu L, Wang YX, Jonas JB. Prevalence of optic disc drusen in an adult Chinese population: the Beijing Eye Study. Acta Opthalmologica 2009;87:227-8.
- Merchant KY, Su D, Park SC, et al. Optic nerve head drusen and visual field loss in normotensive and hypertensive eyes. Ophthalmology 2013;120:1409–14.
- Flores-Rodriguez P, Gili P, Martin-Rios MD. Ophthalmic features of optic disc drusen. Ophthalmologica 2012;228:59-66.
- Pineles SL, Arnold AC. Fluorescein angiographic identification of optic disc drusen with and without optic disc edema. Journal of Neuro-Ophthalmology 2012;32:17-22.
- Gili P, Flores-Rodriguez P, Yanguela J, Orduna-Azcona J, Martin-Rios MD. Sensitivity and specificity of monochromatic photography of the ocular fundus in differentiating optic nerve head drusen and optic disc oedema: optic disc drusen and oedema. Graefes Archive for Clinical & Experimental Ophthalmology 2013;251:923-8.
- Lee KM, Woo SJ, Hwang JM. Morphologic characteristics of optic nerve head drusen on spectral-domain optical coherence tomography. American Journal of Ophthalmology 2013;155:1139-47.e1.
- Hu K, Davis A, O’Sullivan E. Distinguishing optic disc drusen from papilloedema. BMJ 2008;337:a2360.
Tags: flashes, prominent optic disc, raised intracranial pressure, optic disc drusen