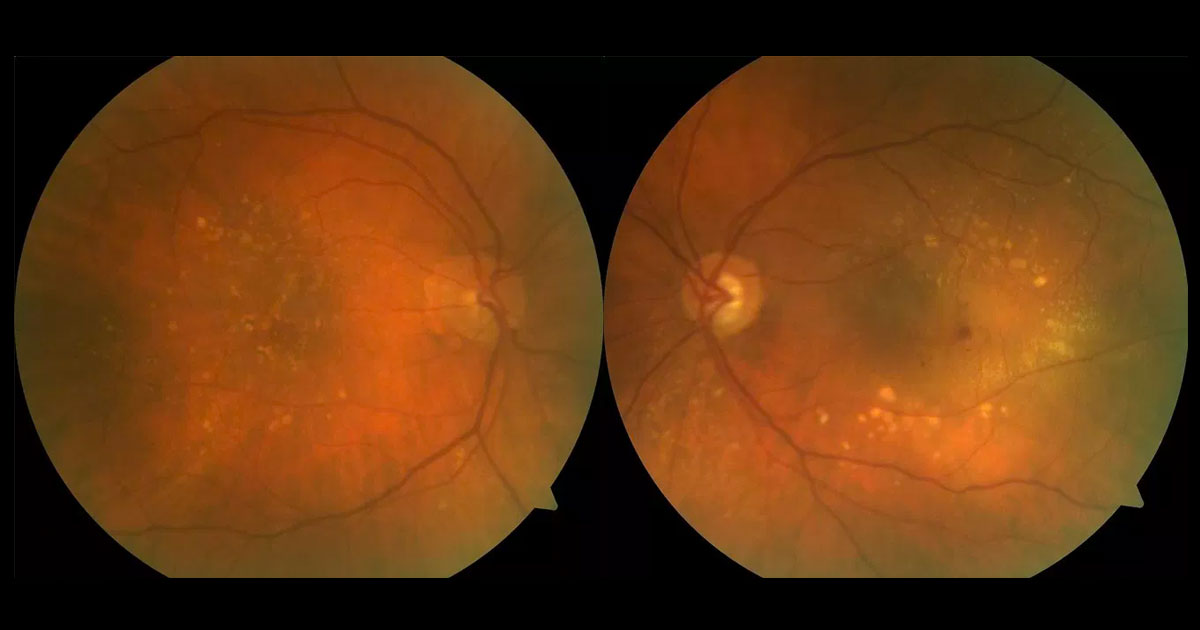
Figure 1. Colour fundus photography of the left eye shows central intra retinal haemorrhage, surrounded by peri-macular soft and hard drusen.
A 66-year old female was referred with blurred vision in her left eye.
A 66-year-old female was referred with blurred vision in her left eye. Visual acuity was 6/7.5 (pinhole no improvement) in the right eye and 6/18 (pinhole no improvement) in the left eye. Moderate nuclear sclerotic and cortical cataracts were present bilaterally. Perifoveal soft and hard drusen were present in both eyes. There was cup disc assymetry with apparent thinning of the neuroretinal rim in the left eye. In the left fundus there was also an intraretinal haemorrhage, subretinal fluid (SRF) and pigment epithelial detachment (PED).
The differential diagnosis for this case includes:
- Age-related macular degeneration
- Type 1 (sub-RPE, including polypoidal choroidal vasculopathy)
- Type 2 (subretinal neovascularisation)
- Type 3 (intraretinal neovascularisation)
- Idiopathic Parafoveal (Macular) Telangiectasia
- Macular branch retinal vein occlusion
- Diabetic retinopathy
Optical coherence tomography (OCT) through the left macula demonstrated intraretinal hyper-reflectance and intra-retinal cysts (white arrow) at the area corresponding to the intraretinal haemorrhage, SRF (green arrow) and a large PED (red arrow) (Figure 2). Fluorescein angiography demonstrated a focal point of intra-retinal hyperfluorescence with feeding arteriole and mild hyperfluorescent leakage. (Figure 3).
Figure 2. Spectral-domain optical coherence tomography at presentation demonstrated an intraretinal hyper-reflective focus and intra-retinal cysts (white arrow) at the area corresponding to intraretinal haemorrhage, subretinal fluid (green arrow) and a large pigment epithelial detachment (red arrow).
Figure 3. Fluorescein angiography demonstrated a focal point of intra-retinal hyperfluorescence with feeding arteriole and mild hyperfluorescent leakage.
DIAGNOSIS
Age-related macular degeneration with left Type 3 neovascularisation.
The patient has received one dose of intravitreal aflibercept with almost complete resolution of the PED and increase of vision by a line to 6/12 (Figure 4). Treatment is ongoing.
Figure 4. Spectral-domain optical coherence tomography one month after a single injection of intravitreal aflibercept, demonstrating dramatic response with resolution of intraretinal cysts, subretinal fluid and pigment epithelial detachment.
Type 3 neovascularisation is recognised as a distinct entity from Gass classification Type 1 (sub-RPE) and Type 2 (sub-retinal) neovascularisation, which usually originates from the choroidal vessels (CNV).(1) There is ongoing debate whether the vascular origin of Type 3 neovascularisation arises from the retinal circulation, choroidal circulation or both.(2) Due to this debate there is a confusing array of descriptors for Type 3 neovascularisation including retinal angiomatous proliferation (RAP), retinal vascular abnormality (RVA) and occult chorioretinal anastomosis (OCA). The term Type 3 neovascularisation avoids the descriptor based on the origin of the lesion and distinguishes it from type 1 and type 2 neovascularisation.
As in our patient, Type 3 neovascularisation commonly presents unilaterally in elderly females, but has a very high rate of subsequent development in the contralateral eye.(3) Clinical findings may include intra-retinal haemorrhages, cystic macular oedema, subretinal fluid and PED. Type 3 lesions always arise from outside the foveal avascular zone, further supporting the hypothesis of an intra-retinal origin.(3)
Classically OCT shows intraretinal hyper-reflectance and cysts extending from the outer plexiform and deeper layers corresponding to the area of angiographic intraretinal neovascularization.(4) Fluorescein angiography demonstrates a focal point of intraretinal neovascularisation that may leak into intraretinal cysts.
The current standard of treatment for type 3 neovascularisation is intravitreal anti-VEGF therapy. In early stages, type 3 neovascularisation has been reported to be highly sensitive to anti-VEGF therapy.(5) Some studies have demonstrated a higher rate of post-treatment retinal pigment epithelial atrophy following anti-VEGF treatment.(6) Other options include photodynamic therapy to the area of intra-retinal neovascularisation.(7)
TAKE HOME POINTS
- Type 3 neovascularization is a distinct form of intraretinal neovascularisation present in a small subset of patients with age-related macular degeneration.
- The site of origin remains debatable, with evidence for both a choroidal and retinal source.
- Presentation is often unilateral in elderly white female patients, although involvement of the fellow eye is common.
- Features include intraretinal proliferating vessels, haemorrhage, cystic oedema. The lesion can penetrate into the subretinal and sub-RPE layers causing a pigment epithelial detachment.
- The intraretinal lesion is most easily seen in the early phases of fluorescein and the serous PED is often not apparent on FA.
- Intravitreal anti-VEGF is currently first-line treatment, although alternative or adjunctive treatment may be considered on a case-by-case basis.
REFERENCES
- Freund KB, Ho IV, Barbazetto IA, et al. Type 3 neovascularization: the expanded spectrum of retinal angiomatous proliferation. Retina 2008; 28: 201–11.
- Freund KB, Zweifel SA, Engelbert M. Do we need a new classification for choroidal neovascularization in age-related macular degeneration? Retina 2010; 30: 1333–49.
- Chapter 11. Adrian T. Fung and K. Bailey Freund (2012). Variants of neovascular age-related macular degeneration: Type 3 neovascularization. Lim AGE-RELATED MACULAR DEGENERATION, Third Edition, p148: Informa healthcare.
- A Rouvas et al. Angiographic and OCT features of retinal angiomatous proliferation. Eye 2010 24, 1633–1643.
- Meyerle CB, Freund KB, Iturralde D, et al. Intravitreal bevacizumab (Avastin) for retinal angiomatous proliferation. Retina 2007; 27: 451–7
- McBain VA, Kumari R, Townend J, Lois N. Geographic atrophy in retinal angiomatous proliferation. Retina 2011; 31: 1043–52.
- Krebs I, Krepler K, Stolba U, Goll A, Binder S. Retinal angiomatous proliferation: combined therapy of intravitreal triamcinolone acetonide and PDT versus PDT alone. Graefes Arch Clin Exp Ophthalmol 2008; 246:237–43.
Tags: blurred vision, intraretinal haemorrhage, age-related macular degeneration, diabetic retinopathy