von Hippel-Lindau disease (VHL) is a highly penetrant, autosomal dominant, multisystem cancer syndrome caused by a germline mutation of the VHL tumour suppressor gene on the short arm of chromosome 3 (3p25–26). About 20% of cases are new mutations, with no family history of the disease. Patients with VHL are at increased risk of developing retinal and central nervous system hemangioblastomas, renal cell carcinomas, pheochromocytomas, neuroendocrine tumors, cysts of the pancreas and endolymphatic sac tumors.(1)
Patient care necessitates a multi-disciplinary approach to regular and lifelong surveillance for ocular and systemic tumours. Well-documented screening protocols are available.(2) It is generally accepted that patients with VHL should have yearly retinal exams from the age of 5 years to screen for RCH. Highly specific and sensitive genetic testing is available to detect patients with the VHL mutation. In addition, antenatal testing is possible.(3)
Retinal capillary haemangioblastomas (RCH) are present in up to 70% of individuals with VHL, and are the most frequent and often the earliest manifestation of the disease. By definition, patients can be diagnosed with VHL if they have:
- More than 1 RCH
- 1 RCH and an associated visceral lesion
- 1 RCH with a family history of VHL.(1)
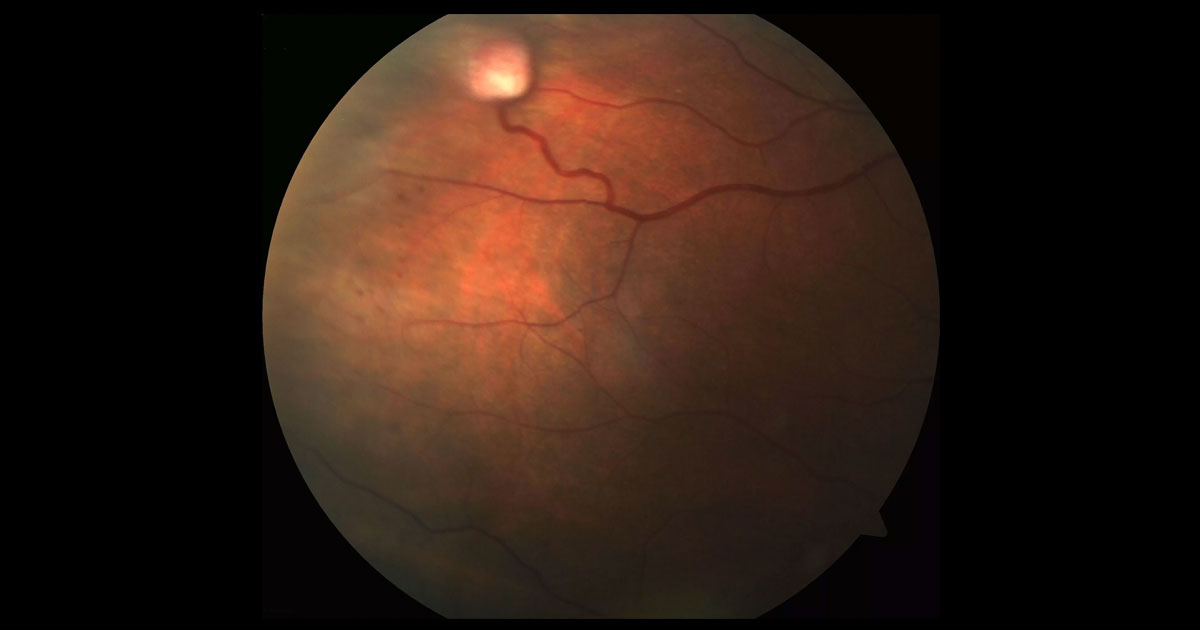
The mean age at diagnosis of RCHs in VHL disease is approximately 25 years, although they can present in the early teens as occurred in our patient. In patients with VHL, RCHs often develop bilaterally, with new lesions developing over time. The lesions are red-colored, highly vascular with a characteristic feeder artery and draining venule. Most commonly the lesions are located in the mid-periphery, however 15% of RCHs occur within one-disc diameter of the optic nerve head.
(4)Although small lesions may remain stable for years, most RCHs associated with VHL tend to progress. Complications including massive exudation, retinal detachment, macula oedema, uveitis, glaucoma and phthisis may occur.
(4) Treatment of RCHs is aimed at tumour ablation in order to prevent further growth and complications. Treatment options for peripheral lesions include laser photocoagulation, cryotherapy, radiation and photodynamic therapy. Laser photocoagulation is used to treat small RCHs in the posterior retina. Ideally the feeder artery is treated first followed by the tumour’s surface.
(5) Cryotherapy is useful for anteriorly located lesions not amenable to laser photocoagulation, or lesions with subretinal fluid.
Lesions of the optic nerve head (juxtapapillary) present a particular treatment challenge. If left untreated, these lesions tend to increase slowly in size over time and ultimately cause exudation and visual loss. Unfortunately, active ablative treatment may cause direct damage to the optic nerve resulting in visual loss. Modalities including photodynamic therapy, proton beam radiotherapy and anti-VEGF agents have been trialed with limited success.
(6)