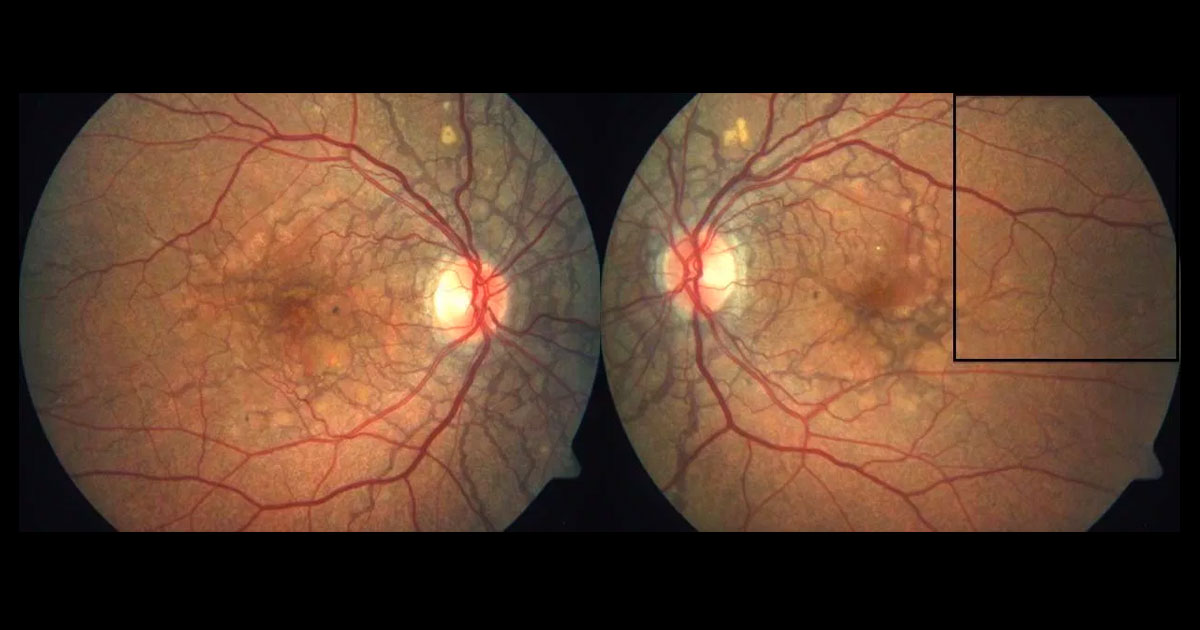
Figure 1a. Fundus photographs reveal bilateral subretinal dark grey concentric and radial lines particularly around the optic nerve heads and maculae.
A 46-year-old Caucasian male saw his optometrist after noticing distortion in his left eye for two months. He was referred with bilateral fundus changes.
A 46-year-old Caucasian male saw his optometrist complaining of a 2-month history of distortion in his left eye. On dilated fundus photography, bilateral dark grey streaks were noted within the posterior poles. He was referred for further assessment.
There was no significant past ophthalmic or medical history. The patient’s brother was known to have an eye condition, but the diagnosis was unknown by the patient. No medications were being taken.
Visual acuity was 6/3.8 in the right eye and 6/9.5+2 (pinhole 6/6) in the left eye. Anterior segments were normal. On fundus examination, bilateral subretinal dark grey concentric and radial lines were noted particularly around the optic nerve heads and maculae (Figure 1). These were identified as angioid streaks. Temporal to both maculae there was a dimpled appearance to the retina, identified as “peau d’orange” (French, “orange peel skin”; Figure 1b).
Figure 1b. Magnified view of the left temporal fundus (rectangle from Figure 1a) reveals “peau d’orange” (French, “orange peel skin”).
The differential diagnosis for angioid streaks includes: idiopathic, pseudoxanthoma elasticum (PXE), Ehlers-Danlos syndrome, Paget’s disease of the bone and sickle cell retinopathy.
Further research into the brother’s ocular condition revealed a family history of PXE. Examination of the patient’s skin revealed waxy papules (“plucked chicken” appearance), especially on the neck (Figure 2).
The angioid streaks could be easily visualised on red free photography (Figure 3) and fundus autofluorescence (Figure 4). Buried optic disc drusen was not present on fundus autofluorescence. On optical coherence tomography (OCT) the streaks were seen as disruptions in Bruch’s membrane with elevations of the retinal pigment epithelium (Figure 5).
Figure 2. Waxy papules (“plucked chicken” skin appearance) was seen on the patient’s neck.
Figure 3. Red free fundus photography highlights the angioid streaks.
Figure 4. Fundus autofluorescence shows the angioid streaks as being hypoautofluorescent. In this patient there is no optic disc hyperautofluorescence, which can indicate the prescence of buried disc drusen.
Figure 5. Optical coherence tomography shows the angioid streaks as disruptions in Bruch’s membrane with elevations of the retinal pigment epithelium.
DIAGNOSIS
Pseudoxanthoma elasticum.
Involvement of the left fovea with an angioid streak was noted on OCT. However, there was no associated haemorrhage, lipid or subretinal or intraretinal fluid suggestive of a choroidal neovascularisation (CNV). The distortion was ascribed to the angioid streak alone and no fluorescein angiography was necessary. The patient was advised to avoid activities that could potentially lead to ocular trauma and to wear safety goggles if playing contact sports. An Amsler grid was provided to monitor for distortion suggestive of CNV. Referrals were made via the patient’s general practitioner to a dermatologist, gastroenterologist and cardiologist to screen for systemic complications associated with pseudoxanthoma elasticum.
Angioid streaks represent calcification and dehiscences of Bruch’s membrane (lying below the retinal pigment epithelium).(1-3) Through these streaks, CNV can grow. This occurs in 76-82% of eyes with angioid streaks, and is bilateral in over 70% of cases.(4) The development of CNV (Figure 6) tends to occur at a younger age than for neovascular age-related macular degeneration and is associated with a thinner than normal choroid.(4) All types of CNV can occur(2) and treatment with intravitreal anti-VEGF agents has been shown to be useful(1,5).
Figure 6. Fundus photograph of the left eye in a patient with angioid streaks secondary to pseudoxanthoma elasticum shows a submacular haemorrhage due to choroidal neovascularisation. This is one of the more common causes for vision in loss in patients with angioid streaks.
The aetiology of angioid streaks is diverse, but can be easily remembered by the pnemonic “PEPSI”:
- Pseudoxanthoma elasticum
- Ehlers-Danlos syndrome
- Paget’s disease of the bone
- Sickle cell disease
- Idiopathic (no detectable systemic association)
Pseudoxanthoma elasticum (PXE OMIM# 264800) is the most common systemic association of angioid streaks, with a reported incidence of 59-87%.
(2) It is an autosomal recessive disorder caused by mutations in the ABCC6 gene with an estimated prevalence of 1 in 50000.
(6) In PXE, elastic fibres undergo calcification and fragmentation. Skin biopsies showing such changes in the dermal layers can assist with confirming the diagnosis.
(7) Organ involvement includes the eyes, skin, cardiovascular and gastrointestinal systems. The combination of eye and skin changes has previously been named Grönbland-Strandburg syndrome.
(2) Common manifestations are outlined below:
(1,3,4,6,8,9)
Eyes- Angioid streaks
- Optic disc drusen
- Peau d’orange
- Peripheral fundus “comets”
- Pattern-like dystrophy
- Choroidal neovascularization
- Geographic atrophy
Skin- Particularly found on flexural skin
- Peau d’orange
- Yellow papules (“plucked chicken” appearance)
- Inelastic skinfolds
Cardiovascular- Accelerated atherosclerosis
Gastrointestinal- Gastrointestinal haemorrhage
Fundus autofluorescence of patients with pseudoxanthoma elasticum is useful in highlighting the streaks and geographic atrophy (both hypoautofluorescent) as well as any buried optic disc drusen (hyperautofluorescent, Figure 7).3
Figure 7. Fundus autofluorescence in a patient with pseudoxanthoma elasticum. The streaks are hypoautofluorescent with hyperautofluorescent stippling. Hyperautofluorescent buried optic disc drusen is present.
Patients with PXE lose vision due to involvement of the fovea by a streak, CNV or geographic atrophy.(2,9) Minor trauma can cause choroidal rupture in patients with PXE and protective goggles are therefore recommended in patients playing contact sports. Systemic involvement may require referral to a physician. Although currently there is no treatment for the underlying ocular or systemic manifestations of PXE, gene therapy may offer the potential of a cure in the future.
TAKE HOME POINTS
- The differential diagnosis of angioid streaks can be remembered by the pnemonic “PEPSI”.
- Ocular signs of pseudoxanthoma elasticum include: angioid streaks, peau d’orange, optic disc drusen (often buried) and peripheral fundus “comets”.
- Vision can be affected by foveal involvement of an angioid streak, choroidal neovascularization or geographic atrophy.
- Angioid streaks complicated by choroidal neovascularisation are often responsive to intravitreal anti-VEGF agents.
- Patients with angioid streaks should be warned that their eyes are more susceptible to damage following blunt ocular trauma. Protective goggles are recommended if patients play contact sports.
- Systemic manifestations of pseudoxanthoma elasticum include: skin changes, ischaemic heart disease and gastrointestinal bleeding.
REFERENCES
- Finger RP, Charbel Issa P, Hendig D, Scholl HP, Holz FG. Monthly ranibizumab for choroidal neovascularizations secondary to angioid streaks in pseudoxanthoma elasticum: a one-year prospective study. American Journal of Ophthalmology 2011;152:695-703.
- Nakagawa S, Yamashiro K, Tsujikawa A, et al. The time course changes of choroidal neovascularization in angioid streaks. Retina 2013;33:825-33.
- Sawa M, Ober MD, Freund KB, Spaide RF. Fundus autofluorescence in patients with pseudoxanthoma elasticum. Ophthalmology 2006;113:814-20.e2.
- Ellabban AA, Tsujikawa A, Matsumoto A, et al. Macular choroidal thickness and volume in eyes with angioid streaks measured by swept source optical coherence tomography. American Journal of Ophthalmology 2012;153:1133-43.e1.
- Shah M, Amoaku WM. Intravitreal ranibizumab for the treatment of choroidal neovascularisation secondary to angioid streaks. Eye 2012;26:1194-8.
- Campens L, Vanakker OM, Trachet B, et al. Characterization of cardiovascular involvement in pseudoxanthoma elasticum families. Arteriosclerosis, Thrombosis & Vascular Biology;33:2646-52.
- Ko JH, Shih YC, Huang YH, Yang CH. Pseudoxanthoma elasticum. Lancet 2013;381:565.
- Goldman DR, Lee GD, Shah CP, Heier JS. Initial presentation of pseudoxanthoma elasticum. JAMA Ophthalmology 2013;131:1352.
- Schoenberger SD, Agarwal A. Geographic chorioretinal atrophy in pseudoxanthoma elasticum. American Journal of Ophthalmology 2013;156:715-23.
Tags: distorted vision, angioid streaks, pseudoxanthoma elasticum, Ehlers-Danlos syndrome