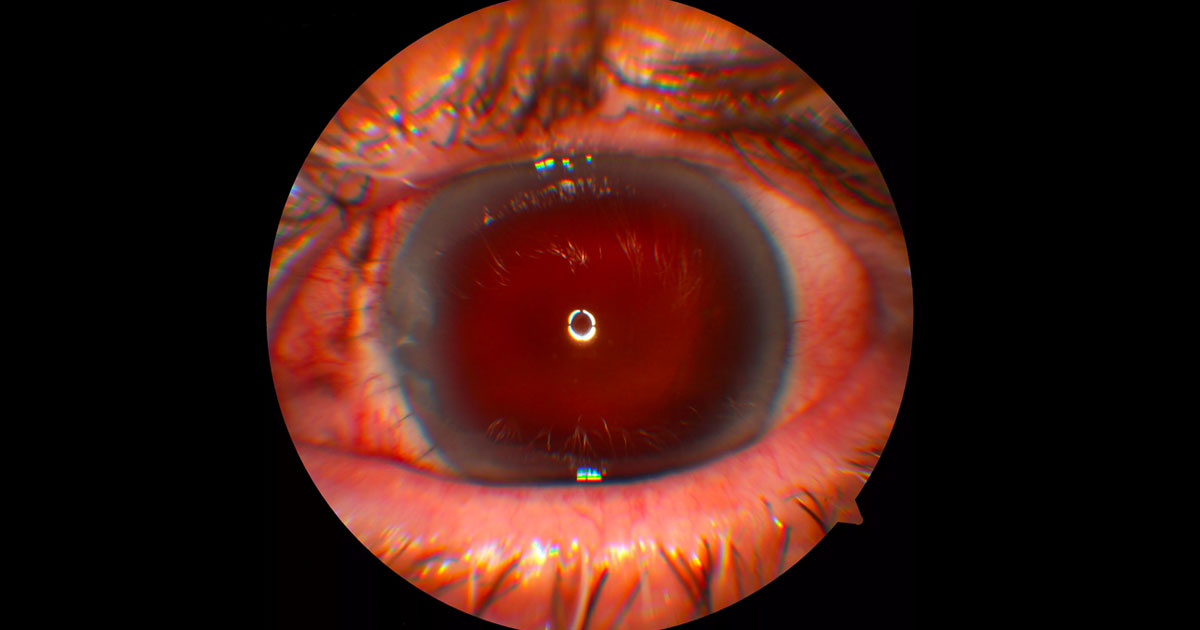
Figure 1. Anterior segment photo of the left eye following primary repair of a globe rupture. The nasal limbal rupture has been closed with interrupted nylon sutures. The eye is aphakic and there is no view of the retina due to a dense vitreous haemorrhage.
A 71-year-old male suffered blunt trauma to his left eye resulting in a globe rupture.
A 71-year-old man was referred by after falling and hitting his left eye on a wooden step. He was found to have a globe rupture, with a large nasal limbal wound and traumatic aphakia and aniridia. Visual acuity was hand motions in the left eye and the intraocular pressure was 3mmHg.
The patient was taken for emergency surgery which involved anterior vitrectomy and closure of the limbal wound with 8-0 nylon suture (Figure 1). Post-operatively he had a dense vitreous haemorrhage and remained hypotonous. At this point (3 weeks post primary globe repair) he was referred for a retinal opinion.
Given the fact that there was no view of the fundus, a B-scan ultrasound was performed. This confirmed the presence of a vitreous haemorrhage, but an unusual splitting of the eye wall was also detected superonasally (Figure 2).
Figure 2. B-scan ultrasonography demonstrates a vitreous haemorrhage and splitting of the eye wall superonasally. The transverse T12 scan looks at the superior retina, with the top of the image nasal. The longitudinal L1030 scan looks from anteriorly at the ciliary body (top of the image) to posteriorly at the optic nerve (bottom of the image) in the 1030 meridian.
The differential diagnosis for a peripheral splitting of the eye wall on B-scan ultrasonography includes:
- Retinal detachment
- Choroidal effusion
- Cyclodialysis cleft and choroidal detachment
- Retinoschisis
DIAGNOSIS
The history of trauma, hypotony and appearance on the B-scan ultrasound is consistent with a cyclodialysis cleft with choroidal detachment.
The patient was followed closely and the vitreous haemorrhage cleared spontaneously by 5 weeks. At this stage the patient remained hypotonous (3mmHg) with corneal oedema, Descemet membrane folds, optic nerve oedema and macular choroidal folds on clinical examination (Figure 3) and OCT (Figure 4).
The patient was referred to a glaucoma specialist who confirmed the presence of a cyclodialysis cleft between 8 and 9 o’clock on gonioscopy. Initially a period of observation was recommended, however 3 months after the injury the eye remained hypotonous despite attempts at medical management with topical atropine and steroids (Maxidex). Repair of the cyclodialysis cleft was therefore performed by fashioning a medial scleral flap, identifying the cleft and suturing it closed with 10-0 nylon. The flap and conjunctiva was closed with 8-0 vicryl.
Nine months after the initial injury with the cyclodialysis cleft successfully repaired, the vision had returned to 6/60 ph 6/9 with an IOP of 19mmHg. The macular choroidal folds had largely resolved (Figure 5). Vision remained poor due to traumatic aphakia.
Figure 3. Colour montage photograph of the left eye shows choroidal folds at the macula due to hypotonous maculopathy.
Figure 4. Optical coherence tomography of the left macula shows choroidal folds due to hypotony.
Figure 5. Following repair of the cyclodialysis cleft, the intraocular pressure normalised and the choroidal folds resolved.
Figure 6. Colour photographs of the right and left eyes. The right eye is normal. The left eye has a Morcher Type 68 Intraocular lens that has been sutured internally to the sclera. This intraocular lens has a prosthetic iris.
A cyclodialysis cleft occurs when the meridional fibres of the ciliary muscle disinsert from the scleral spur(1). This may be a result of blunt external trauma or following intraocular surgery. The cleft allows for direct flow of aqueous humour from the anterior chamber to the ciliochoroidal space and often results in hypotony. The hypotony may cause complications including shallowing of the anterior chamber, cataract, optic nerve oedema, choroidal effusions and choroidal folds with hypotonous maculopathy. Cyclodialysis clefts can be visualised by gonioscopy, ultrasound biomicroscopy (UBM) and anterior segment OCT.
Initial medical management includes atropine to relax the ciliary body.(2) Topical steroids have been described as having a positive(2) or negative(1) effect on cyclodialysis clefts. Surgical treatment of cyclodialysis clefts is indicated when hypotony persists leading to ocular complications. Many options are possible, and include argon laser photocoagulation, transscleral diode photocoagulation, cryotherapy, diathermy, translimbal and transsceral suturing, scleral buckling, vitrectomy and intravitreal gas tamponade.(3)
Options for surgical placement of an intraocular lens includes insertion into the capsular bag, sulcus, anterior chamber, iris clip or suture and scleral suture or tunnelling. When the capsular bag and iris are not present such as following trauma, only a scleral fixated IOL is possible. Prosthetic irides are indicated for aniridia, both for cosmetic reasons and to reduce glare. Companies that manufacture this include Morcher (Stuttgart, Germany), Ophtec (Groningen, Germany) and HumanOptics (Erlangen, Germany). The prosthetic iris may be separate from, or part of the IOL. Recently, use of CV-8 GORE-TEXÒ suture instead of Prolene to fixate the IOL has been thought to give greater longevity. The use of Hoffman pockets avoids the need for scleral flaps.
TAKE HOME POINTS
- A cyclodialysis cleft occurs when the ciliary muscle fibres disinsert from the scleral spur, allowing direct communication between the anterior chamber and suprachoroidal space.
- Scleral fixation of intraocular lenses are required when the capsular bag and iris are missing. Prosthetic iris implants may be used to treat aniridia and reduce glare
- Cyclodialysis clefts usually result from external trauma or intraocular surgery
- Complications of cyclodialysis clefts arise from the resultant hypotony.
REFERENCES
- Ioannidis A, Barton K. Cyclodialysis cleft: causes and repair. Curr Opin Ophthalmol 2010; 21:150-154.
- Romano MR, Vinciguerra R, Randazzo A, Vinciguerra P. Management of Cyclodialysis Clef Associated to hypotonic maculopathy. Graefes Arch Clin Exp Ophthalmol. 2013; 251:1023-1024.
- Malandrini A, Balestrazzi A, Martone G, Tosi GM, Caporossi A. Diagnosis and Management of Traumatic Cyclodialysis Cleft. J Cataract Refract Surg 2008; 34:1213-1216.
Tags: fundus lesion, normal vision, haemangioblastoma, retinoblastoma