Case 55
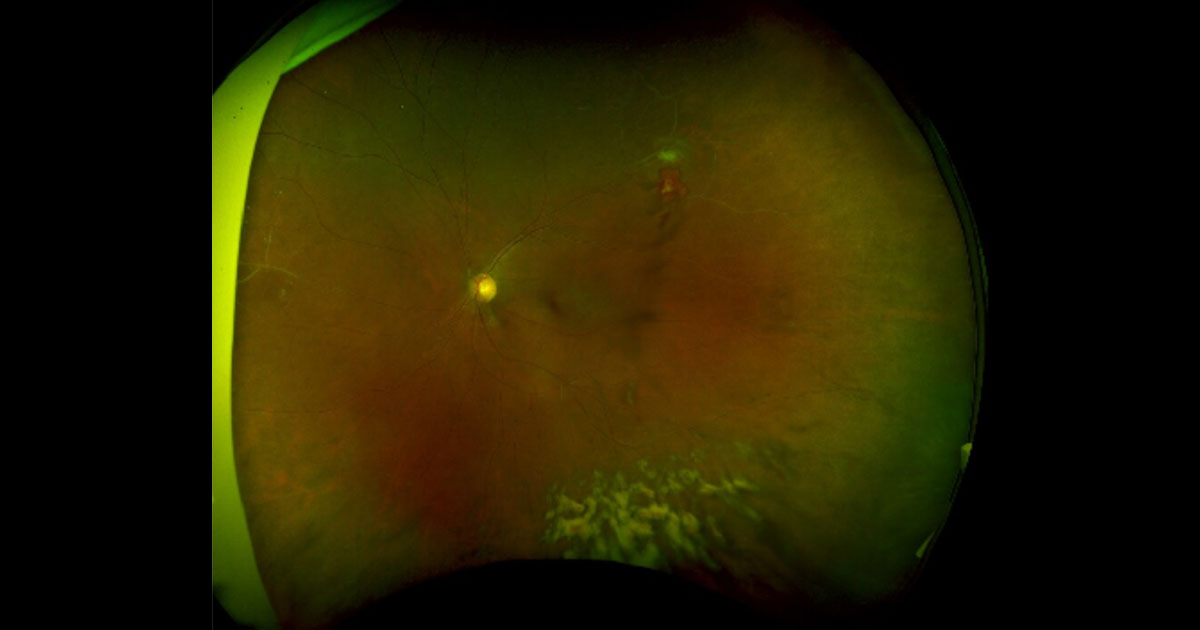
Figure 1. Vitreous haemorrhage was noted inferiorly in this wide view colour photo of the left eye. There is an area suspicious of neovascularisation supero-temporally, as well as evidence of sclerosed retinal vessels in the periphery.
Author: Amy Pai Editor: Adrian Fung
A 36-year-old Caucasian male was referred with headache, orbital pain, vertigo and blurred vision.
Case history
A 44-year-old man presented to his optometrist complaining of 3 days of seeing black spots in his left vision, which is not improving with time. He has never experienced anything similar in the past and denied any previous ocular problems. He has diet controlled Diabetes and does not take any regular medications normally. He denied past or recent trauma, intervention or ocular surgery. He does not wear glasses normally. He denied a family history of eye problems, and feels that his central vision is still good despite the ‘black spots’. He denied smoking.
Visual acuity was 6/5 unaided in both eyes. Intraocular pressures and pupil reactions were normal. Dilated exams revealed no evidence of cataracts, and no inflammatory cells in the anterior chamber in either eye. There was no evidence of iris nodules or keratic precipitates (KPs). There was evidence of vitreous haemorrhage in his left eye whereas the right vitreous was clear. An area suspicious of neovascularisation was noted supero-temporally on his left retina (Figure 1) and there was also evidence of sclerosed blood vessels nasally and supero- temporally. His right fundus appeared normal (Figure 2). There was no evidence of cystoid macular oedema or macular changes in either eye.

Figure 2. Right colour fundus photo showing no acute changes.



