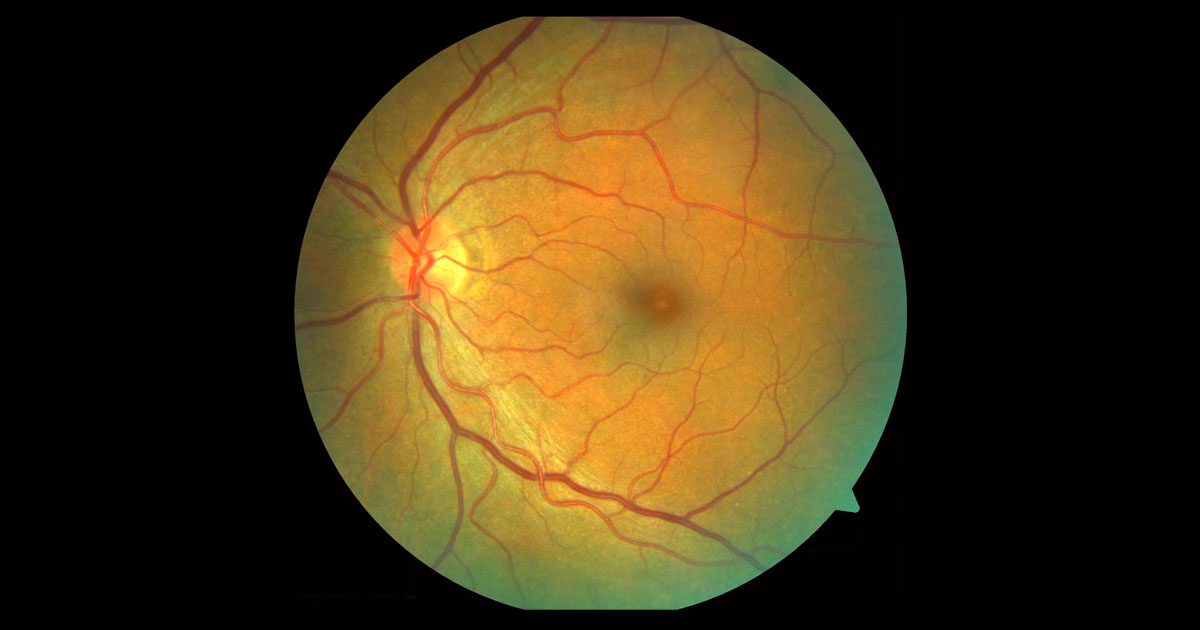
Figure 1. Colour fundus photograph of the left eye demonstrates a yellow spot at the fovea.
A 65-year-old male was referred with left reduced visual acuity and macular changes.
A 65-year-old Caucasian male was referred with a 1-week history of reduced vision and mild metamorphopsia in his left eye. He had previously had a corneal foreign body but there was no other significant past ocular or medical history. There was no history of significant ocular trauma.
Visual acuity was 6/6 in the right eye (OD) and 6/24 (pinhole 6/12) in the left eye (OS). Intraocular pressures were normal and the anterior segment examination unremarkable. Examination of the left macula demonstrated a yellow spot at the fovea (Figure 1). The right macula was normal. Optic nerves were healthy with cup to disc ratios of 0.2 bilaterally. A few fine drusen were present bilaterally but there was no other significant pathology in either eye.
Figure 1b. Magnified view of the left temporal pigmented lesion.
The differential diagnosis of a yellow spot at the fovea includes:
- Vitreomacular Traction Syndrome (VMTS)
- Macular hole
- Cystoid macular oedema
- Adult foveomacular vitelliform dystrophy
- Solar maculopathy
- Recreational laser retinopathy
- Alkyl Nitrite ‘Popper’ retinopathy
Optical coherence tomography (OCT) demonstrated a very small full thickness macular hole (Figure 2).
Figure 2. Left optical coherence tomography demonstrates a full thickness retinal disruption at the fovea. Note the rounded edges and overlying operculum. The posterior hyaloid has detached off the macula.
DIAGNOSIS
Left full thickness macular hole (FTMH).
The clinical findings and diagnosis were discussed with the patient. The options of observation (given the very small size of the hole) and surgery were discussed. He opted for initial close observation and two weeks later reported less distortion with a slight improvement in vision (6/12 pinholing 6/9-2 OS) . The yellow spot was less evident on clinical examination and the OCT scans demonstrated improvement particularly of the inner retina (Figure 3). At 6 weeks after his initial presentation the left visual acuity had improved to 6/7.5. Further improvement of the foveal architecture with restoration of the outer retina layers was seen on OCT (Figure 4).
Figure 3. Left optical coherence tomography at 2 weeks. Note the continuity of the foveal contour and ‘bridging’ of the inner retina with persistent disruption of the outer retinal layers.
Figure 4. Left optical coherence tomography at 6 weeks. Note the restoration of the outer retina including the external limiting membrane and photoreceptors.
Idiopathic full thickness macula holes are a relatively common macular condition typically occurring in patients over 60 years with a slight female predominance. Spectral domain OCT imaging has added to the understanding of the pathophysiology, which is thought to be due to vitreomacular traction. Traditional clinical staging1 has now been replaced by OCT staging2 (Table 1):
Table 1. Staging of Macular Holes
| Traditional clinical staging |
International Vitreomacular Traction Study Classification |
|
Stage 0: |
VMA |
|
Stage 1: Impending macular hole |
VMT |
|
Stage 2: Small hole |
Small to medium FTMH with VMT |
|
Stage 3: Large hole |
Medium to large FTMH with VMT |
|
Stage 4: FTMH with PVD |
FTMH without VMT |
FTMH: Full thickness macular hole, PVD: Posterior vitreous detachment , VMA: Vitreomacular adhesion, VMT: Vitreomacular traction. NB: “Small” ≤250 μm, “Medium” 250-400 μm, “Large” >400 μm. Modified from Duke JS, Kaiser PK, Binder et al. The International Vitreomacular Traction Study Group Classification of Vitreomacular Adhesion, Traction and Macular Hole. Ophthalmology 2013;120:2611-2619.
Impending or Stage 1 holes, which are characterised by vitreomacular traction (VMT) and an inner foveal cyst, are known to have a 50% chance of spontaneous resolution and can be observed.(2) In contrast, spontaneous closure of FTMH is rare (2.7-3.5%).(3,4,5) Most FTMHs require surgery involving pars plana vitrectomy, internal limiting membrane peeling and gas. This operation has a high rate of successful closure and a corresponding improvement in visual acuity. Pharmacologic vitreolysis is not an option when there is no VMT, as in this case.
This case documents the rare spontaneous resolution of a FTMH. Close initial observation was considered an appropriate option given the very small size of the hole with almost opposing edges, and the recent onset. If no change was seen at the 2 week follow-up, vitrectomy surgery would have been recommended. The 2 week OCT image (Figure 3) demonstrates a ‘bridging’ process of the inner retina that has been previously documented in similar cases of spontaneous closure.(4,6)
Most cases of macular holes present unilaterally, with bilateral holes occurring in 11.7% of patients.(7) In unilateral cases it is important to discuss the risk of macular hole development in the contralateral eye, the incidence of which has been reported to be 5-16%. It is much less frequent in eyes where there is a posterior vitreous detachment. In our case there was clear separation of the posterior hyaloid at the right fovea on OCT scans (Figure 5). This allowed the patient to be reassured that a macular hole was unlikely to occur in his right eye.
Figure 5. Right optical coherence tomography demonstrating separation of the vitreous from the fovea.
TAKE HOME POINTS
- Most full thickness macular holes require vitrectomy surgery for closure.
- Spontaneous closure of a full thickness macular hole is rare.
- ‘Bridging’ of the inner retinal layers is an early finding in cases of spontaneous closure.
- Patients can be reassured that they are unlikely to develop a macular hole in their contralateral eye if the hyaloid is seen to have already detached off the fovea on optical coherence tomography scans.
REFERENCES
- Gass JD. Reappraisal of biomicroscopic classification of stages of development of a macular hole. Am J Ophthalmol. 1995;119:752-759.
- Duke JS, Kaiser PK, Binder et al. The International Vitreomacular Traction Study Group Classification of Vitreomacular Adhesion, Traction and Macular Hole. Ophthalmology 2013;120:2611-2619.
- La Cour M, Friis J. Macular holes: classification, epidemiology, natural history and treatment. Acta Ophthalmol Scand. 2002;80:579-587.
- Sugiyama A, Imasawa M, Chiba T, Iijima H. Reappraisal of Spontaneous Closure Rate of Idiopathic Full-Thickness Macular Holes. The open Ophthalmology Journal. 2012:6: 73.
- Privat E, Tadayoni R, Gaucher D, Haouchine B, Massin P, Gaudric A. Residual defect in the foveal photoreceptor layer detected by optical coherence tomography in eyes with spontaneously closed macular holes. Am J Ophthalmol. 2007;143:814–9.
- Hamano R, Shimoda Y, Kishi S. Tomographic features of spontaneous closure of full-thickness macular holes. Jpn J Ophthalmol. 2007; 51(1):76-7.
- McCannel CA, Ensminger JL, Diehl NN, et al . Population-based incidence of macular holes. Ophthalmology 2009:116:1366-9.
Tags: reduced visual acuity, yellow foveal spot, vitreomacular traction sydrome, macular hole