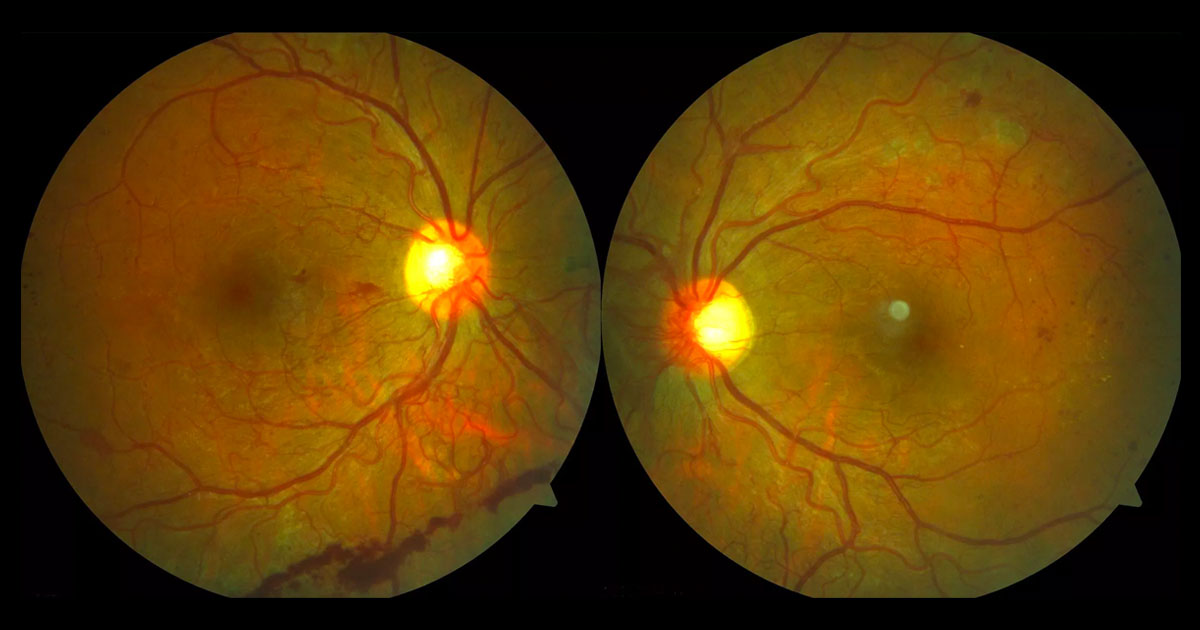
Figure 1A. Colour fundus photographs showing bilateral neovascularization at the optic discs and “elsewhere”, intraretinal microvascular abnormalities (IRMAs) and microaneurysms. Pre-retinal haemorrhage is seen inferiorly in the right eye and scattered fine hard exudates in the left eye.
A 22-year-old mother was referred after noticing new floaters in her right eye.
A 22-year-old mother (6 months postpartum) was referred after noticing floaters in her right eye. She also reported difficulty with her night vision and adjusting to dim illumination.
Past medical history included type 1 insulin dependent diabetes mellitus (IDDM) diagnosed at the age of 5 years. She admitted to poor glycaemic control as a teenager and during her recent pregnancy. Uncertain of her most recent HbA1c, the patient acknowledged her current blood sugar levels (BSL) were far from optimal. There was no known history of hypertension, hyperlipidaemia or renal impairment. Past ocular history included previous poorly tolerated retinal laser treatment but no prior intravitreal injections or surgery.
On examination visual acuities were 6/7.5 pinholing to 6/6 bilaterally. Intraocular pressures were normal. There was no neovascularisation of the iris or angles and the lenses were clear. Posterior segment examination demonstrated extensive new vessels at the disc and “elsewhere”, intraretinal microvascular abnormalities (IRMAs) and microaneurysms in both eyes. (Figure 1A and 1B). In the right eye there was associated pre-retinal and mild vitreous haemorrhage. In the left temporal macula scattered hard exudates were noted without significant associated retinal thickening. A moderate degree of panretinal photocoagulation laser scars were present bilaterally in the retinal peripheries.
Figure 1B. Magnified view of the left optic disc showing neovascularization (“new vessels”).
With a known diagnosis of longstanding poorly controlled insulin dependent diabetes mellitus, this case does not present a diagnostic challenge with the findings representing active proliferative diabetic retinopathy (PDR).
In the absence of a known history of diabetes mellitus, diabetic retinopathy would be the provisional diagnosis. Other possible causes of neovascularisation in the posterior segment include:
- Retinal vascular occlusions
- Ocular ischaemic syndrome
- Radiation retinopathy
- Sickle cell retinopathy
- Retinopathy of prematurity
Optical coherence tomography (OCT) scans of the maculae were obtained. There was no evidence of diabetic macular oedema in the right eye. In the left eye temporal macula hard exudates were evident as hyperreflective deposits but there was minimal intraretinal fluid (Figure 2). Fundus fluorescein angiography confirmed the clinical findings of active PDR (Figure 3).
Figure 2. Optical coherence tomography of the left macula demonstrates mild intraretinal fluid spaces temporally and hyperreflective deposits consistent with hard exudates.
Figure 3. Fundus fluorescein angiography shows hyperfluorescent leakage from new vessels at both optic discs and along the right inferotemporal vascular arcade. Hyperfluorescent microaneurysms are most prominent temporally where there is capillary dropout. The foveal avascular zones of both eyes are irregular. Blocked fluorescence from pre-retinal hemorrhage is seen inferiorly in the right eye. Panretinal photocoagulation laser marks are seen superotemporally in the left eye.
DIAGNOSIS
Proliferative diabetic retinopathy.
The clinical findings and diagnosis of proliferative diabetic retinopathy were discussed with the patient. Her treatment options were outlined including the benefits and potential risks of further panretinal photocoagulation (PRP) laser. It was emphasised that the goal of treatment was to reduce her risk of vision loss. To assist with improving her metabolic control the patient was referred to a diabetic clinic.
In light of previously poorly tolerated laser, prompt bilateral fill-in PRP laser was arranged under general anaesthesia. One month after fill-in PRP laser the patient reported a drop in her vision. Her right visual acuity measured 6/9 and left visual acuity 6/12. Repeat OCT imaging demonstrated bilateral macular oedema (Figure 4).
Figure 4. Optical coherence tomography scans show cystic oedema at the right fovea and temporal to the left fovea.
The right eye was injected with intravitreal bevacizumab (Avastin®) with resolution of the macular oedema and an improvement of vision to 6/7.5. Modified focal laser was applied to the left temporal macula but the development of a left vitreous haemorrhage dropped the vision to hand motions. When the blood failed to clear the patient underwent left intravitreal bevacizumab (Avastin®) followed by pars plana vitrectomy. The surgery involved segmentation and delamination of the posterior hyaloid and residual diabetic fibrovascular tissue, endolaser fill-in PRP laser and subtenon triamcinolone.
Eight months after initial presentation the patient’s visual acuity has improved to 6/7.5 bilaterally. The neovascularisation has regressed with resolution of the diabetic macular oedema (Figures 5 and 6). Additionally her glycaemic control has gradually improved.
Figure 5. Colour fundus photographs demonstrating regression of the new vessels following peripheral panretinal photocoagulation. Note the peripheral laser scars.
Figure 6. Optical coherence tomography scans showing resolution of the macular oedema following right intravitreal bevacizumab (Avastin®) injection and left focal macular laser.
Proliferative diabetic retinopathy (PDR) represents an advanced stage of diabetic eye disease and if left untreated has a significant risk of profound vision loss. It is characterised by the formation of new vessels at the optic nerve and on the retina. The presence of preretinal haemorrhage should alert the clinician to look carefully for neovascularisation. In severe cases new vessels can also grow on the iris and in the angle, causing rubeotic glaucoma. Angiogenesis is stimulated by retinal ischaemia and hypoxia leading to the production of pro-angiogenic factors such as vascular endothelial growth factor (VEGF).(1)
Almost all patients with type 1 diabetes mellitus will develop some degree of retinopathy within 20 years of onset. The rate of progression is related to blood sugar level control and blood pressure.(2) Progression of diabetic retinopathy is also known to occur with pregnancy,(3) but may regress in the postpartum period.(5)
Panretinal laser photocoagulation (PRP) is the mainstay of treatment of PDR, reducing the risk of severe vision loss by at least 50%.(6,7) Potential side effects of PRP laser include reduced peripheral vision, poorer night vision and exacerbation of macular oedema.(8) In ideal circumstances existing diabetic macular oedema is addressed prior to the administration of PRP, but this is not always possible in cases of severe PDR.
The role of intravitreal anti-VEGF agents such as bevacizumab (Avastin®) in diabetic retinopathy is expanding. They are now first line for treatment of diabetic macular oedema,9 and is often used in conjunction with focal macular laser. They also have a role in the context of PDR(10) when administered to reduce intraoperative and postoperative vitreous hemorrhages(11) or for the treatment of neovascular glaucoma.
TAKE HOME POINTS
- Proliferative diabetic retinopathy (PDR) represents advanced diabetic eye disease with high risk of profound visual loss.
- The main signs include new vessels at the disc and “elsewhere” in the retina. The presence of preretinal haemorrhage should alert the clinician to look for these.
- Risk factors for progression of diabetic retinopathy include poor glycaemic control, hypertension and pregnancy.
- The mainstay of treatment of PDR is panretinal photocoagulation (PRP) laser.
- Side effects of PRP include reduced peripheral or night vision and exacerbation of macular oedema.
- Intravitreal anti-VEFG agents are first-line in the management of diabetic macular oedema.
- Intravitreal anti-VEGF agents may also be useful in patients with PDR such as prior to diabetic vitrectomy surgery.
REFERENCES
- Antonetti DA, Klein R, Gardner TW. Diabetic Retinopathy. New England Journal of Medicine 2012;366:1227-39.
- Klein R, Knudson MD, Lee KE, et al. The Wisconsin Epidemiologic Study of Diabetic Retinopathy XXII. The Twenty-Five-Year Progression of Retinopathy in Persons with Type 1 Diabetes Ophthalmology 2008;115(11):1859-68.
- Klein BE, Moss SE, Klein R. Effect of pregnancy on progression of diabetic retinopathy. Diabetes Care 1990;13:34-40.
- Che Ey, James LM, Metzger BE. Diabetes in Early Pregnancy Study Group. Diabetes Care 1995;18:631-7.
- Serup L. Influence of pregnancy on diabetic retinopathy. Acta Emdpcromp; 1986;13:165-9.
- Photocoagulation treatment of proliferative diabetic retinopathy. Clinical application of Diabetic Retinopathy Study (DRS) findings, DRS Report Number 8; The Diabetic Retinopathy Study Research Group. Ophthalmology 1981;88:583-600.
- Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 1991;98:766-785.
- Fong DS, Girach A, Boney A. Visual side effects of successful scatter laser photocoagulation surgery for proliferative diabetic retinopathy: a literature review. Retina 2007 Sep;27(7):816-24.
- Virgili G, Parravano M, Menchini F, Evans JR. Anti-vascular endothelial growth factor for diabetic macular oedema. Cochrane Database Syst Rev. 2014 Oct 24;10:CD007419.
- P Osaadon, X J Fagan, T Lifshitz and J Levy. A review of anti-VEGF agents for proliferative diabetic retinopathy. Eye 2014;28:510-520.
- Zhang ZH, Liu HY, Hernandez-Da Mota SE, et al. Vitrectomy with or without preoperative intravitreal bevacizumab for proliferative diabetic retinopathy: a meta-analysis of randomized controlled trials. American Journal of Ophthalmology 2013 Jul;156(1):106-115.
Tags: floaters, pregnancy, diabetic retinopathy, neovascularisation