A 68-year old man was referred with profound vision loss one day following cataract surgery.
A 68-year-old retired accountant was referred by his ophthalmologist with profound vision loss noted on the first day following right femtosecond laser assisted cataract surgery. The patient had sub-Tenon’s anaesthesia and there had been no documented intraoperative complication.
Past ophthalmic history was only notable for myopia with a preoperative refraction of –1.50/ -1.00x 91° (right eye) and -0.25/ -1.25 x 86° (left eye). Past medical history included recently diagnosed Parkinson’s disease treated with Sifrolâ (pramipexole) and hypercholesterolaemia treated with Pravacholâ (pravastatin). There was no history of smoking or previous cardiovascular events such as stroke or heart attack.
Visual acuity was hand movements (HM) OD and 6/7.5-1 OS. There was a right relative afferent pupil defect suggesting optic nerve or diffuse retinal pathology. Eye movements and lid opening were full and there was no subconjunctival or periocular haemorrhage nor exophthalmos to suggest a retrobulbar haemorrhage. The cornea was clear with no significant corneal oedema, and ½+ anterior chamber cells were noted. The intraocular lens was in the bag and well centred. There was a grade 2 nuclear and cortical cataract in the left eye. Intraocular pressures were 14mmHg OD and 16 mmHg OS.
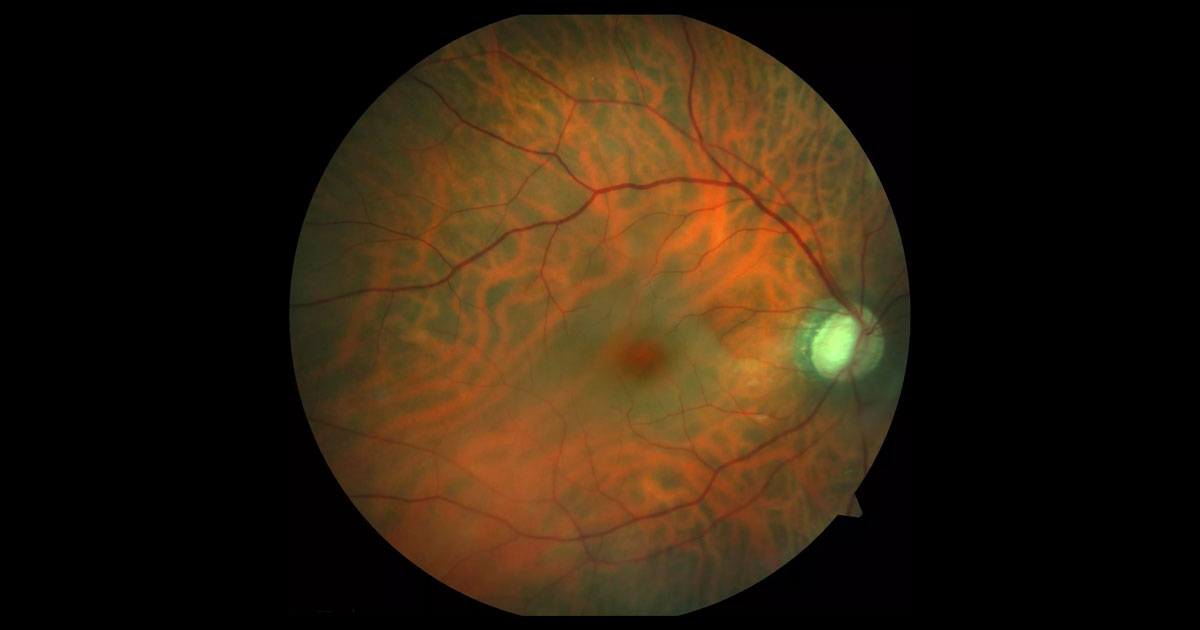
Fundus examination of the right eye demonstrated a pale retina with cherry red spot at the macula (Figure 1). The cup disc ratio was enlarged at 0.8 OD and 0.6 OS. The retinal arterioles appeared attenuated (Figures 1 and 2). Myopic scleral crescents were present bilaterally. No emboli were seen in either eye.
Figure 2. Red free imaging of the right fundus demonstrates arterial attenuation. No retinal emboli are seen.
The differential diagnosis for a cherry red spot following cataract surgery includes:
- Central retinal artery occlusion
- Retinal toxicity from intraoperative gentamicin use
Optical coherence tomography (OCT) through the right macula demonstrated hyper-reflectivity within the inner retinal layers (Figure 3). This was not evident in the left macula. A mild epiretinal membrane was also present. Fluorescein angiography (FFA) demonstrated moderately delayed arterial filling (Figure 4). No emboli were visualised, consistent with a central retinal artery occlusion.
Further discussion with the surgeon confirmed that no gentamicin was used intra-operatively, but intracameral cephazolin was used at the end of the case. There were no symptoms of giant cell arteritis (GCA). Specifically, the patient did not report jaw claudication, temporal and scalp tenderness, headache, neck stiffness or systemic malaise. Carotid Doppler studies did not demonstrate significant carotid stenosis. His heart rate was regular and there were no signs of atrial fibrillation.
Figure 3. Right optical coherence tomography (horizontal raster scan) through the macula at presentation demonstrates increased reflectivity localized to the inner retina. A mild epiretinal membrane is present.
Figure 4. Right fundus fluorescein angiography. There was a mild delay in arm to retina time and arterial filling. There are no retinal emboli.
DIAGNOSIS
Right central retinal artery occlusion (CRAO) following femtosecond laser assisted cataract surgery.
At review one month later the visual acuity remained at hand movements only. The cherry red spot had resolved as had most of the retinal oedema and pallor. The retinal arterial system remained attenuated and the optic disc was pale. There was no anterior segment neovascularisation. The left eye remains healthy apart from some cataract.
Figure 5. Right colour fundus photograph one month after presentation. There has been resolution of the cherry red spot. Some retinal oedema and whitening still persists. The retinal arterioles are attenuated and the disc is pale.
Central retinal artery occlusion (CRAO) is a rare and devastating complication following cataract surgery. This is the first reported case in the setting of femtosecond laser assisted cataract surgery.
The mechanism for CRAO in the setting of cataract surgery is uncertain.(1,2) It is felt most likely to be related to the anaesthetic block either by a vasospastic effect of the anaesthetic on the central retinal artery (CRA), by a secondary increase in intraocular pressure (IOP) causing occlusion of the artery or by increasing the intraorbital pressure such that it causes compression of the CRA as it passes through the orbit.(1,2)
Anaesthetic agents can act as vasoconstrictors, even in the absence of adrenaline, and could have a vasoconstrictive effect on the CRA that might result in occlusion. Findl et al.(3) have reported that lignocaine and bupivacaine reduce retinal blood flow velocity by 15% and 10% at 1 and 5 minutes, respectively, after peribulbar anaesthesia without adrenaline.
Increased IOP secondary to compression on the globe by the anaesthetic agent or intra-operative manoeuvres might also cause CRAO.(2) The retinal vessels however have a good autoregulatory capacity over a wide range of perfusion pressures, meaning that a transient change in IOP is unlikely to contribute sufficiently to the decreased retinal perfusion enough to cause a CRAO.(2) This is the first reported case of CRAO in the setting of femtosecond laser assisted cataract surgery, however the use of the femtosecond laser is likely to be coincidental. Although docking of the laser platform does raise the IOP, this rise is only temporarily in the order of +10mmHg4 and as discussed the IOP rise required to cause a CRAO is likely to be much higher and more prolonged than this. Additionally, the CRA perfusion pressure is much higher than the central retinal vein so if the IOP mechanism were likely one would anticipate a higher proportion of central retinal vein occlusion (CRVO).
The third potential mechanism would be due to a mechanical effect of the anaesthetic volume on the central retinal artery.(2) Increased intraorbital pressure might be sufficient to compress the CRA as it passes through the orbit.
Unfortunately, as discussed in our Case of the Month July 2014, the visual prognosis for CRAO is poor with only 10% of patients reporting meaningful recovery of vision.(5) Patients still need to be observed for iris and angle neovascularisation which can occur in up to 1/3 of patients.(6) The onset of neovascularisation in CRAO is often one to two months following occlusion as opposed to the traditional 90 days in CRVO.
When the patient comes to requiring cataract surgery in the fellow eye, topical or general anaesthesia in an effort to avoid peribulbar or sub-Tenon’s anaesthesia should be considered given the potential mechanisms discussed.
TAKE HOME POINTS
- Central retinal artery occlusion following otherwise uncomplicated cataract surgery is a rare but devastating event. This is the first reported case in the setting of femtosecond laser assisted cataract surgery.
- The putative mechanisms relate to the local anaesthetic block either due to: a vasoconstrictive effect on the central retinal artery, a rise in intraocular pressure or a pressure effect on the central retina artery as it passes through the orbit.
- The cause of a pale retina and cherry red spot following cataract surgery is likely to be either a CRAO or retinal toxicity from gentamicin.
REFERENCES
- Vinerovsky A, Rath EZ, Rehany U, Rumelt S. Central retinal artery occlusion after peribulbar anaesthesia.Journal of Cataract & Refractive Surgery 2004, 30: 913-5.
- Swamy BN, Merani R, Hunyor A. Central retinal artery occlusion following phacoemulsification.Retinal Cases & Brief Reports 2010; 4: 281–283.
- Findl O, Dallinger S, Menapace S et al.Effects of peribulbar anesthesia on ocular blood flow in patients undergoing cataract surgery.Am J Ophthalmol, 1999, 127: 645–649
- Kerr NM, Abell FG, Vote BJ, Toh T’. Intraocular pressure during femtosecond laser pretreatment of cataract. J Cataract Refract Surg 2013; 39:339–342
- Rumelt S, Dorenboim Y, Rehany U. Aggressive systematic treatment for central retinal artery occlusion. Am J Ophthalmol 1999; 128: 733–738.
- Rudkin AK, Lee AW, Chen CS. Ocular neovascularisation following central retinal artery occlusion: prevalence and timing of onset. Eu J Ophthalmol 2010; 20: 1042–1046.
Tags: vision loss, cataract surgery, central retinal artery occlusion, retinal toxicity