Case 43
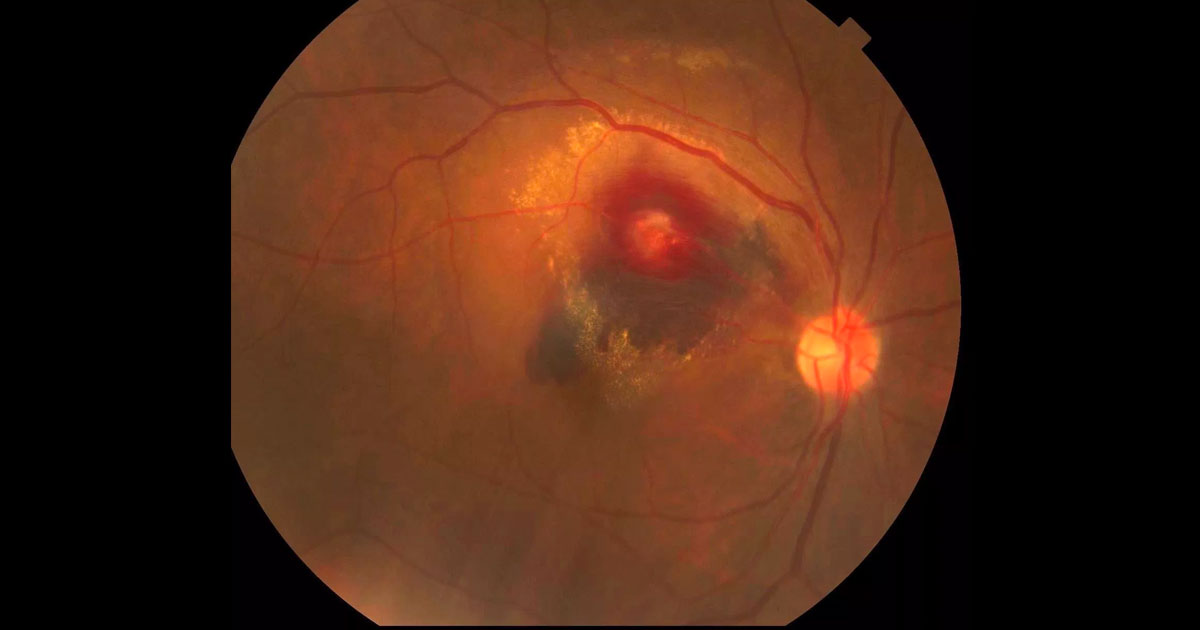
Figure 1. Colour photograph of the right eye at presentation demonstrating a multilayered haemorrhage and hard exudate involving the macula.
Author: Michael Chilov Editor: Adrian Fung
A 72-year-old woman was referred with acute painless vision loss in her right eye.
Case history
A 72-year-old lady was referred by her optometrist complaining of a one day history of a scotoma involving the central vision of her right eye.
She had no previous ophthalmic history and had not seen an optometrist for a number of years. Her past medical history included hypertension, previous transient ischaemic attack (TIA) and hypercholesterolaemia. Her medications included aspirin, perindopril/indapamide (Coversyl Plus) and simvastatin (Zocor). She was a previous smoker having stopped more than 15 years previously.
Visual acuity was counting fingers (CF) in the right eye (OD) and 6/9+ in the left eye (OS). There was no relative afferent pupil defect (RAPD). Examination of the right fundus (Figure 1) revealed a multilayered retina haemorrhage, with darker subretinal haemorrhage in the inferior part involving the macula, and superficial nerve fibre layer haemorrhage more superior to this. There was a small amount of vitreous haemorrhage inferiorly. In the centre of the haemorrhage was a paler area. Hard exudate was present surrounding the haemorrhagic region and tracking towards the macula.
There were chronic hypertensive retinal vascular changes with AV nipping and copper wiring. There was no disc swelling. In the left eye, aside from similar chronic hypertensive changes, the retinal examination was unremarkable.
Grade 3+ nuclear sclerotic cataracts were present bilaterally. Intraocular pressures were OD 18mmHg and OS 17 mmHg.



